Early systolic deceleration vertebral artery (ESDV VA) is a hemodynamic phenomenon characterized by a decrease in vertebral artery blood flow velocity during early systole. This unique and intriguing phenomenon offers valuable insights into the complex interplay between intracranial pressure (ICP) and cerebral hemodynamics, making it an essential consideration in neurocritical care.
ESDV VA has emerged as a non-invasive marker of elevated ICP, providing clinicians with a crucial tool for assessing cerebral perfusion and guiding therapeutic interventions. However, it is essential to understand the limitations of ESDV VA as a diagnostic tool and the potential pitfalls associated with its interpretation.
Pathophysiology of Early Systolic Deceleration Vertebral Artery
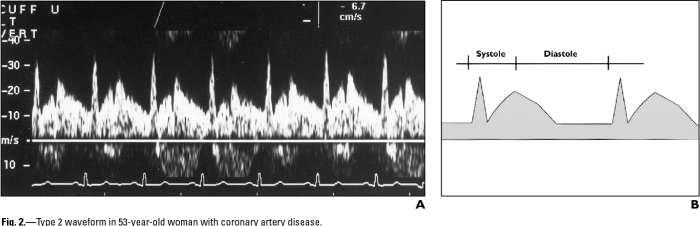
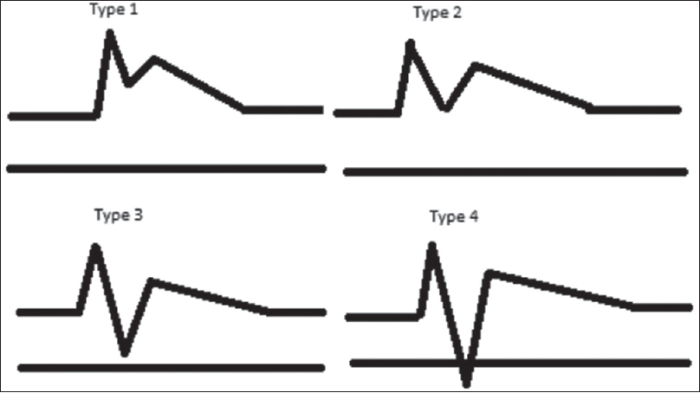
Early systolic deceleration vertebral artery (ESDV VA) is a hemodynamic phenomenon characterized by a decrease in the velocity of blood flow in the vertebral artery during early systole. This abnormality is associated with increased intracranial pressure (ICP) and is thought to be caused by a reduction in cerebral perfusion.
Increased ICP can lead to a decrease in the diameter of the vertebral artery, which in turn reduces the velocity of blood flow. This decrease in blood flow can be detected using transcranial Doppler (TCD) ultrasound, which is a non-invasive technique that measures the velocity of blood flow in the cerebral arteries.
Anatomical Structures Involved in ESDV VA, Early systolic deceleration vertebral artery
The vertebral artery is a major artery that supplies blood to the posterior circulation of the brain. It originates from the subclavian artery and ascends through the transverse foramina of the cervical vertebrae. The vertebral arteries join together at the level of the foramen magnum to form the basilar artery, which supplies blood to the brainstem and cerebellum.
The vertebral artery is located in close proximity to the brainstem and cerebellum, which are both sensitive to changes in ICP. Increased ICP can cause the brainstem and cerebellum to herniate, which can compress the vertebral artery and reduce blood flow to the posterior circulation.
Clinical Significance of ESDV VA
ESDV VA is a clinically significant finding that is associated with increased ICP and decreased cerebral perfusion. It is a non-invasive marker of elevated ICP that can be used to guide therapy and monitor the response to treatment.
ESDV VA has been shown to be a predictor of poor outcome in patients with head injury, subarachnoid hemorrhage, and other conditions that are associated with increased ICP. It is also a useful tool for monitoring the response to ICP-lowering therapies, such as osmotherapy, hyperventilation, and cerebrospinal fluid drainage.
However, it is important to note that ESDV VA is not a specific marker of increased ICP. It can also be caused by other factors, such as arterial stenosis or dissection. Therefore, it is important to interpret the findings of ESDV VA in the context of the patient’s clinical presentation and other diagnostic tests.
Methods for Detecting ESDV VA
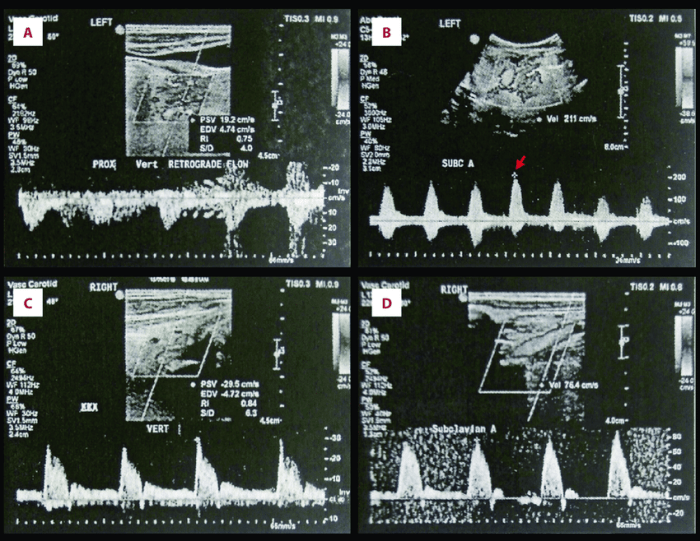
ESDV VA can be detected using TCD ultrasound. TCD is a non-invasive technique that measures the velocity of blood flow in the cerebral arteries. The TCD probe is placed on the temporal bone and is used to insonate the vertebral artery.
The velocity of blood flow in the vertebral artery is then measured using the Doppler effect.
There are different methods for measuring ESDV VA using TCD. The most common method is the pulsatility index (PI), which is a measure of the difference between the peak systolic and end-diastolic velocities. Other methods for measuring ESDV VA include the resistive index (RI) and the Gosling pulsatility index (GPI).
| Method | Advantages | Disadvantages |
|---|---|---|
| Pulsatility index (PI) | Simple to measure | Not as sensitive as RI or GPI |
| Resistive index (RI) | More sensitive than PI | More difficult to measure |
| Gosling pulsatility index (GPI) | Most sensitive method | Most difficult to measure |
Management of ESDV VA
The management of ESDV VA is aimed at reducing ICP and improving cerebral perfusion. This can be achieved through a variety of therapeutic interventions, including:
- Osmotherapy: Osmotherapy involves the administration of hypertonic solutions, such as mannitol or hypertonic saline, to reduce ICP.
- Hyperventilation: Hyperventilation involves increasing the rate of ventilation to reduce ICP.
- Cerebrospinal fluid drainage: Cerebrospinal fluid drainage involves the removal of cerebrospinal fluid from the ventricles or subarachnoid space to reduce ICP.
The choice of therapeutic intervention will depend on the underlying cause of the ESDV VA and the patient’s clinical condition.
In patients with head injury, the initial management of ESDV VA typically involves osmotherapy and hyperventilation. If these measures are not effective, then cerebrospinal fluid drainage may be necessary.
In patients with subarachnoid hemorrhage, the management of ESDV VA typically involves osmotherapy and cerebrospinal fluid drainage. Hyperventilation is not typically used in this setting, as it can increase the risk of vasospasm.
The following flowchart Artikels the management algorithm for patients with ESDV VA:
- Assess the patient’s clinical condition and determine the underlying cause of the ESDV VA.
- Initiate osmotherapy and hyperventilation.
- If osmotherapy and hyperventilation are not effective, then consider cerebrospinal fluid drainage.
- Monitor the patient’s clinical condition and adjust the treatment plan as necessary.
Question & Answer Hub
What is the clinical significance of ESDV VA?
ESDV VA is a non-invasive marker of elevated ICP, providing valuable information about cerebral perfusion and guiding therapeutic interventions in neurocritical care.
How is ESDV VA detected?
ESDV VA is detected using transcranial Doppler (TCD) ultrasound, a non-invasive technique that measures blood flow velocity in the vertebral artery.
What are the limitations of using ESDV VA as a diagnostic tool for ICP monitoring?
ESDV VA can be affected by factors other than ICP, such as arterial stiffness and blood pressure, which can limit its accuracy as a diagnostic tool.